Minimally Invasive Circumcision
The Most Refined Technique with Minimal Tissue Damage
Microsurgical circumcision is a minimally invasive procedure that combines an innovative dual local anesthesia technique, providing stable and long-lasting anesthesia to effectively reduce discomfort during and after surgery. Using microsurgical-level precision, only excessive foreskin is accurately removed while preserving the underlying subcutaneous tissue as much as possible. This minimizes damage to blood vessels and nerves, results in minimal bleeding, and promotes faster wound healing. The incision line follows a natural oblique oval contour, achieving a more proportionate length and a smooth, natural postoperative appearance. Compared with other surgical methods, microsurgical circumcision offers a shorter recovery time and less postoperative discomfort, making it a modern option that balances safety, comfort, and aesthetics.

Precision Microsurgical Excision

Dual Anesthesia for Stable Pain Control

Minimal Bleeding • Faster Recovery

Natural Incision Line • Smooth Appearance

Comparison Table of Circumcision Methods
| Surgical Method | Microsurgical Circumcision | Laser Circumcision | Circumcision Stapler | Traditional Circumcision |
|---|---|---|---|---|
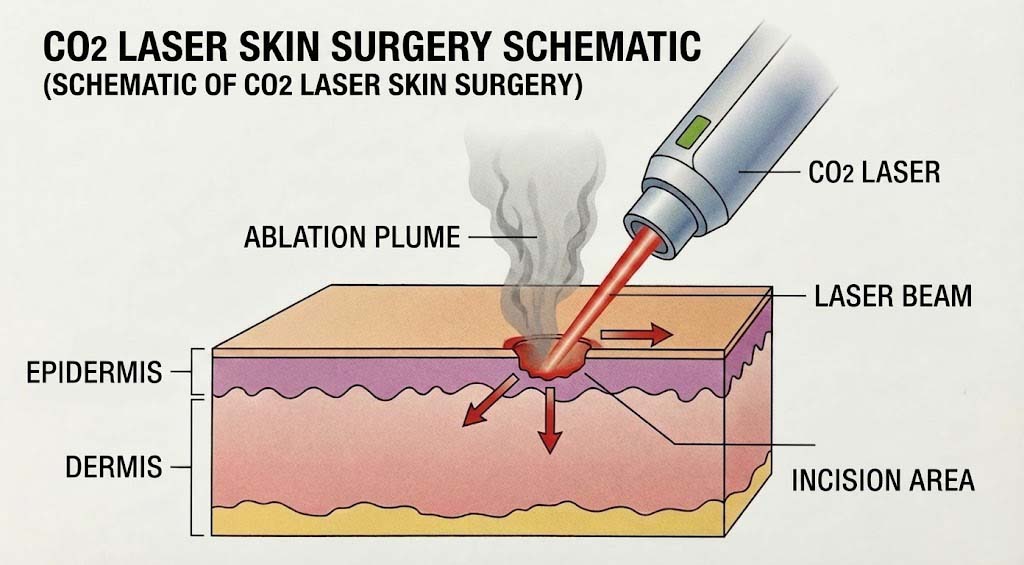
| Technical Principles | Microsurgical precision techniques with low-temperature cold-blade incision | CO2 laser high-temperature vaporization and cutting | Mechanical simultaneous cutting and staple fixation | Scalpel incision combined with electrocautery hemostasis |
| Anesthesia Method (Duration) | Dual local anesthesia (4–6 hours) | Standard local anesthesia (30–60 min) | Standard local anesthesia (30–60 min) | Standard local anesthesia (30–60 min) |
| Wound Shape | Oblique oval (parallel to the glans contour) | Circular or Oblique-oval | Circular | Circular or Oblique-oval |
| Impact on Tissue Vitality | Minimal: Precisely avoids nerves, lymphatics, and blood vessels | Moderate to high: High-thermal effect may cause thermal injury to surrounding tissues | Moderate to high: Removes more healthy subcutaneous tissue (indicated in red) | high: Electrocautery charring often leads to a lack of blood supply in local tissues |
| Hemostasis Method | Ligation with absorbable fine sutures | Laser high-temperature coagulation hemostasis | Staple compression hemostasis | Electrocautery hemostasis |
| Pain Level | Lower: Better postoperative pain improvement | Slightly higher: Possible burning sensation post-surgery | Slightly higher: Potential discomfort during staple shedding | Higher: More pronounced postoperative swelling |
| Operation Time | 60–90 minutes | 30–40 minutes | 20–30 minutes | 30–60 minutes |
| Potential Complications | Very low tissue injury | Slightly higher: Potential thermal injury, delayed wound healing | Slightly higher: Potential asymmetry in foreskin length, occasional difficulty in staple shedding, and staples may not secure firmly in thicker skin | Higher: Hematoma, edema, tissue injury, delayed wound healing |
| Recovery time | Faster: Sutured with fine non-absorbable monofilament; sutures removed after one week | Slower: Requires time for charred tissue to metabolize and repair | Slower: Requires 14–21 days for staple shedding | Slower: Susceptible to inflammation and edema |
Why Choose Microsurgical Circumcision?
Derived from traditional circumcision techniques and further refined using microsurgical principles1, this procedure is performed with the patient in a supine position. A novel dual local anesthesia technique is applied to the deeper penile structures and surrounding areas, eliminating the risks associated with general anesthesia while extending anesthesia duration to 4–6 hours2. Patients remain awake and pain-free during surgery, can use mobile devices or listen to music, and are able to walk home immediately after the procedure without postoperative observation.
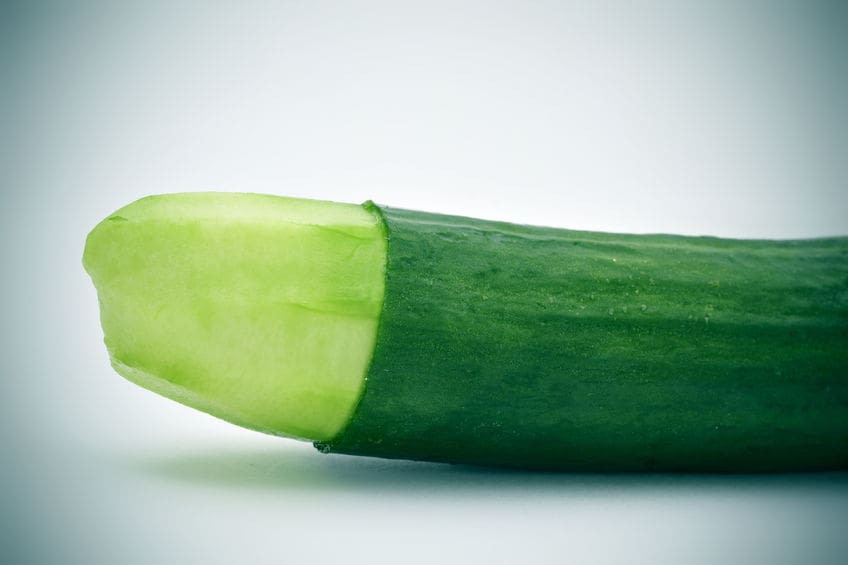
The incision line follows the natural oblique oval contour of the glans(Fig.1A). Since the dorsal foreskin is longer and the ventral foreskin shorter, this tailored design ensures symmetry, improved cosmetic outcomes, and avoids excessive ventral skin removal that could cause tension or pain during erection or intercourse due to pulling on the scrotal skin.
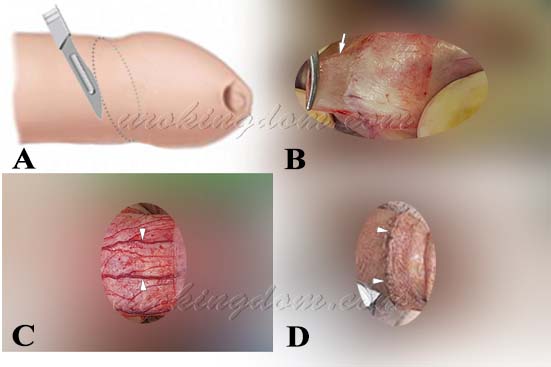
Only a thin superficial layer of foreskin is removed (Fig.1B). Bleeding is extremely minimal, and electrocautery is not used for hemostasis during microsurgical circumcision. Any minor bleeding points are managed with fine absorbable sutures, preventing damage to underlying tissues, vessels, and nerves (Fig.1C). This preserves more subcutaneous tissue with minimal damage and facilitates faster healing. Wound closure is performed using fine non-absorbable monofilament sutures that are removed after one week, resulting in minimal inflammation and rapid recovery; or fine absorbable sutures that will gradually fall off one week after surgery (Fig.1D).
Numerous medical studies have shown that electrocautery can damage local tissues, reduce blood supply, impair resistance to infection, and delay wound healing3. It also has the potential to injure nearby penile arteries and nerves, which can lead to:
- Sensory abnormalities
- Numbness
- Ischemic necrosis (tissue death due to lack of blood flow)
- Erectile dysfunction
Surgical Technique Overview
Figure 1. The microsurgical circumcision begins with natural oblique oval incision made below the glans:
- A) The incision line run parallel to the oblique oval contour of the glans, resulting in a more natural and aesthetically pleasing appearance.
- B) Only a very thin superficial layer of foreskin was removed.
- C) The underlying tissues and blood vessels were preserved, minimizing tissue damage.
- D) Using delicate suturing techniques, the wound was closed precisely. At the one-week postoperative follow-up, the superficial skin layer showed excellent healing.
Key Advantages of Microsurgical Circumcision

- Extended anesthesia duration with improved postoperative pain control
- Single incision, no hospitalization, no general anesthesia risk
- Natural oblique oval incision for better cosmetic results
- No electrocautery, minimal tissue damage, faster healing
- Enhanced surgical safety with reduced complication rates
- Improved hygiene and reduced risk of balanitis Lower risk of sexually transmitted infections4
Conclusion
Microsurgical Circumcision minimizes damage to neurovascular tissues, ensuring a faster recovery, more proportionate skin length, and superior aesthetic outcomes. This approach is significantly safer and associated with fewer complications. In addition to microsurgical circumcision, our clinic applies these same core principles—prioritizing safety and minimizing complication rates—to all other procedures, including:
- subinguinal microsurgical varicocelectomy
- microsurgical hernia repair
- refined penile venous surgery
- penile curvature correction
- penile prosthesis implantation
- testicular prosthesis implantation
- microsurgical no-scalpel vasectomy
- dorsal penile nerve block surgery
Surgical Precaution
- Active balanitis must be treated medically prior to surgery
- Diabetic patients should ensure good blood sugar control
- Pain is minimal during surgery due to prolonged anesthesia
- No hospitalization required
- Post-op discomfort can be managed with anti-inflammatory medications
- Some discomfort from nocturnal erections may occur on the first night
- Normal daily activities can usually be resumed immediately after surgery.
- Smoking and secondhand smoke may impair wound healing and should be avoided.
Microsurgical circumcision offers safety, low complication rates, and better cosmetic results among all circumcision methods. Always consult a qualified urologist to determine the best approach for your needs.
Various Circumcision & Traditional circumcision

Both lasers and circumcision staplers are convenient surgical cutting tools, each with its own set of advantages and disadvantages. Because these methods are not suitable for everyone, a thorough and careful evaluation by a professional urologist is essential before undergoing surgery.
Traditional circumcision
Using traditional local anesthesia methods, two parallel circular incisions are made at appropriate positions below the coronal sulcus of the glans. With the aid of a scalpel, the excess prepuce (foreskin) and subcutaneous tissue between these two incisions are dissected and removed. After the excision, electrocautery is used for hemostasis, and the wound is closed with absorbable sutures.
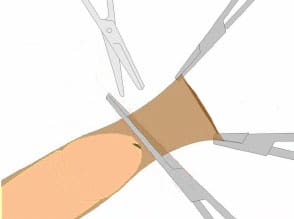
There are also many variations of this technique, such as the ‘tug-and-chop’ method (Figure 4), which emphasizes simplicity and speed. Because traditional circumcision does not place a strong emphasis on delicate precision, it can easily damage underlying tissues, blood vessels, and nerves. This may lead to postoperative complications such as:
- Bruising or swelling at the surgical site
- Hematoma (internal bleeding/bruising)
- Edema (swelling)
- Infection and inflammation
- Poor wound healing
- Penile numbness (loss of sensation)
- Cold sensation in the glans
- Erectile dysfunction
- Urethrocutaneous fistula (abnormal connection between the urethra and skin)
- Excessive foreskin removal, causing tension or pain during erection or intercourse due to pulling on the scrotal or lower abdominal skin
When Should Circumcision Be Considered?
- Recurrent balanitis/balanoposthitis or urinary tract infections
- History of paraphimosis
- Phimosis and Sexual Trauma: When the penis is erect, if the opening of the foreskin is relatively narrow and cannot be retracted below the coronal sulcus, surgery is generally recommended.
- Diabetic complications: Patients present with poor peripheral circulation and foreskin may appear pale, cracked, swollen, and prone to chronic infection.
- Concurrent Lesions: If there are other pathological lesions on the redundant foreskin, such as condyloma acuminatum (commonly known as genital warts or “cauliflower warts”), concurrent surgical excision may be considered.
- Hygiene and Odor: An excessively long foreskin makes it difficult to maintain proper hygiene, which often leads to persistent and annoying odors.
- Prevention of sexually transmitted infections (STI): Circumcision can reduce the risk of contracting STIs, including Human Immunodeficiency Virus (HIV), Human Papillomavirus (HPV), Herpes Simplex Virus type 2 (HSV-2), and syphilis4.
Remark
Redundant foreskin is defined as a condition where the prepuce entirely covers the glans penis in its flaccid state, preventing the glans from being exposed naturally; however, the foreskin remains manually retractable for hygiene and cleansing. This condition is clinically distinct from phimosis. In phimosis, the preputial orifice is pathologically narrow, rendering it impossible to retract the foreskin to expose the glans. During micturition (urination), urine may stagnate within the preputial sac, causing a phenomenon known as preputial ballooning.
When Is Circumcision Not Necessary?
- Newborns without medical or religious indication
- Penile developmental anomalies (e.g., hypospadias)
- Pediatric phimosis responsive to steroid ointment
- Buried penis due to obesity (weight control preferred)
References
- Geng-Long Hsu、Cheng-Hsing Hsieh. Book:A LABORATORY MANUAL FOR POTENCY MICROSURGERY, Geng-Long Hsu and Cheng-Hsing Hsieh, eds
- Hsu GL, Hsieh CH, Chen HS, Ling PY, Wen HS, Liu LJ, Chen CW, Chua C. The advancement of pure local anesthesia for penile surgeries: can an outpatient basis be sustainable? Journal of Andrology. 28(1):200-205, 2007.
- Hsu GL, Hsieh CH, Wen HS, Hsu WL, Chen YC, Chen RM, Chen SC, Hsieh JT. The effect of electrocoagulation on the sinusoids in the human penis. Journal of Andrology. 25(6):954-9, 2004.
- Yang SSD, Hsieh CH, Chang SJ. Effects of circumcision on urinary tract infection and sexually transmitted disease. Tzu Chi Medical Journal. 21(3):185-189, 2009.
Frequently Asked Questions
Microsurgical minimally invasive circumcision is an advanced surgical technique that utilizes microsurgical-level precision combined with dual local anesthesia. It allows for accurate removal of excessive foreskin while preserving as much underlying tissue, nerves, and blood vessels as possible. Compared with traditional circumcision methods, this technique results in less bleeding, faster healing, and a more natural cosmetic outcome.
The main differences include:
✔ Microsurgical precision minimizes damage to nerves and blood vessels
✔ No electrocautery is used, reducing the risk of thermal tissue injury
✔ The incision follows the natural oblique oval contour of the glans for better cosmetic results
✔ Longer-lasting anesthesia with less postoperative pain
✔ Shorter recovery time and lower risk of inflammation and complications
The procedure uses dual local anesthesia, which typically lasts 4–6 hours. Patients remain awake during the procedure but should not feel pain. Many patients are able to use their phone or listen to music during surgery. Postoperative discomfort is usually mild and manageable with prescribed pain medication.
No.
Microsurgical circumcision is performed as an outpatient procedure using only local anesthesia, eliminating the risks associated with general anesthesia. Patients can walk independently and return home shortly after the procedure without the need for hospital admission.
The incision is designed along the natural oblique oval contour of the glans, allowing for better symmetry and a smooth, natural appearance. Because tissue trauma is minimal and suturing is fine and precise, visible scarring is usually minimal.
Most patients can expect:
✔ Immediate return to light daily activities
✔ Suture removal or natural suture dissolution in about 7 days
✔ Superficial wound healing within approximately 7–10 days
✔ Avoid strenuous exercise and sexual activity for 2–4 weeks
Recovery time may vary depending on individual healing and postoperative care.
Each method has its own advantages and limitations:
🔥 Laser circumcision: High temperatures may cause thermal damage to surrounding tissues and slower healing
🔫 Stapler circumcision: Faster procedure time, but less symmetry and requires time for staple removal
🔬 Microsurgical circumcision: Minimal tissue damage, natural appearance, and faster recovery
The most suitable option should be determined by a qualified physician after proper evaluation.
