Circumcision generally means that the foreskin encases the entire penis and glans, and the glans cannot be exposed naturally; however, when washing, the foreskin can usually be flipped over and removed to reveal the glans. Circumcision is different from circumcision. The foreskin is too tight in front of the foreskin, so the foreskin cannot be flipped over and removed to reveal the glans. Urine tends to accumulate in the foreskin cavity during urination, causing the foreskin to expand like a ballooning. Recent studies have shown that circumcision can reduce the risk of acquiring sexually transmitted diseases, including human immunodeficiency virus (HIV), human papillomavirus (HPV), herpes type 2 virus (type 2 HSV) and syphilis (syphilis).
Methods of circumcision

Circumcision Anastomosis
There are many different methods of circumcision, including traditional circumcision, laser circumcision, circumcision anastomosis (circumcision gun) (Figure 1), and the newer microcircumcision. Laser circumcision has the advantage of less bleeding because it stops bleeding at the same time as laser cutting; circumcision anastomosis has the advantage of simultaneous cutting and stapling and short operation time, but the cost is higher due to the fixed cost of the equipment.
Traditional circumcision
Using the traditional local anesthesia method, the foreskin is cut in two parallel circular wounds at an appropriate location below the coronal sulcus of the glans, and the foreskin and subcutaneous tissue between the two wounds are cut with the assistance of a scalpel. There are also many variations, such as the tug-and-chop method (Figure 2), which emphasizes its simplicity and speed.
Traditional circumcision does not place special emphasis on delicate surgery, which can easily injure the underlying tissues, blood vessels, and dorsal nerve plexus, resulting in postoperative complications such as wound bruising and swelling, poor healing, and penile numbness.
Possible complications of traditional circumcision
Bruising and swelling of the wound.
Inflammation of the wound.
Poor wound healing.
Numbness of the penis.
Cold sensation of the glans.
Erectile dysfunction.
Urethral skin fistula.
Too much circumcision and pain or injury caused by pulling the scrotum or lower abdominal skin during erection or sexual intercourse.
The glans feels more sensitive at first after surgery and usually adapts soon afterwards.
Microcircumcision
Derived from traditional circumcision and modified, the procedure is performed using microsurgical techniques.
An innovative method of local anesthesia is applied to the deep part of the penis and the surrounding area in a lying position.
the penis and the surrounding area in a lying position. Two shallow, thin, parallel circumcision wounds (Figure A, B) are made below the coronal groove of the glans, leaving the subcutaneous tissues and blood vessels uninjured. C), preserving the underlying tissue and blood vessels.
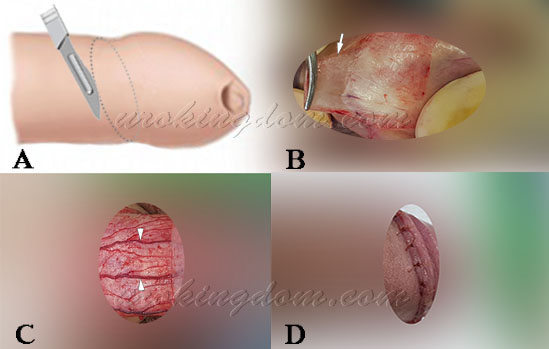
In case of small bleeding spots during the procedure, instead of using electrocautery to stop bleeding, absorbable microscopic sutures are used to tie the wound to stop bleeding, and the wound is finally closed with absorbable microscopic sutures (Figure D).
A. A shallow, thin, oblique oval wound was cut at an appropriate location on the foreskin covering the glans (right lateral view)
B. The foreskin is retracted to expose the coronal sulcus, and another shallow and thin circumferential wound is cut at an appropriate location, and the wound near the coronal sulcus is clamped with fine mosquito forceps and peeled to remove the foreskin, removing only a shallow and thin layer of foreskin (white arrow)
C. Subcutaneous size vessels are clearly visible (white arrow), uninjured and bleeding, preserving the tissue beneath it (top view)
D. The wound is closed with absorbable microfine sutures (right side view), and the suture threads will gradually fall off after the wound can be touched with water for one week after surgery.
The delicate surgery removes only a thin layer of foreskin, preserving the largest amount of subcutaneous tissue and avoiding injury to the tissue, blood vessels and nerves underneath, with minimal bleeding. Since the penis is not large and the blood vessels and nervous system are quite close, the use of electrocautery to stop bleeding during surgery may injure the immediately adjacent dorsal penile artery, dorsal nerve plexus or surrounding tissues, causing abnormal nerve sensation, numbness, local ischemic necrosis of the remaining foreskin or erectile dysfunction (impotence).
In addition, many medical literature reports have pointed out that when using electrocautery to stop bleeding, the local tissues are damaged and there is no blood circulation to the burnt area to stop bleeding, which will increase the chance of wound inflammation and infection; even if there is no inflammation and infection, it will easily affect the wound healing.
Microcircumcision does not require the use of electrocautery to stop bleeding at all, with minimal destruction of tissues such as nerves and blood vessels and minimal bleeding, which is the safest method with the least amount of sequelae. Not only circumcision, but we perform the rest of the related penile surgeries, including penile vein amputation, penile curvature correction, and artificial penile implantation, all following this principle to minimize the chance of complications.
The benefits of microcircumcision are and?
- The innovative double local anesthesia is effective for a long time and lasts until several hours after the procedure.
- The procedure is performed using microsurgical techniques and takes approximately one hour.
- The foreskin is cut in an oblique oval shape, with the most precise and appropriate length.
- Tissues such as nerves and blood vessels are minimally disrupted and normal tissue structures are preserved.
- Bleeding is minimal and no electrocautery is used to stop bleeding.
- The incision is flat and neat, and the wound heals smoothly and beautifully.
- Maintain local cleanliness and hygiene.
- Reduce the incidence of glansitis.
- Reduce the risk of acquiring sexually transmitted diseases.
What are the precautions for microcircumcision?
- The acute phase of glans penis requires medication to control the inflammation and wait for the inflammation to subside before surgery.
- A very small number of people are allergic to local anesthetics.
- The innovative double local anesthesia method is used, and the effective anesthesia lasts about 4 to 6 hours. The procedure is painless and can last until several hours after the surgery. After the anesthesia has worn off, the surgical wound inevitably feels painful and uncomfortable, and postoperative pain can be relatively reduced by starting to take anti-inflammatory pain medication after surgery. On the first night after surgery, nocturnal penile erection during sleep can be uncomfortable, but usually after the next day, the wound will gradually become more comfortable and painless, and you can immediately perform your daily tasks without hospitalization.
- Smoking or secondhand smoke will affect wound healing and tissue recovery and should be avoided at all costs.
- Occasionally, there may be slight bleeding from the wound, bruising on the ventral side of the glans or under the skin, and edema of the foreskin after surgery, which will usually subside and resolve on its own.
- The wound should be kept dry for 7 days after surgery and should not be wetted by water. Return to the clinic 2 to 3 days after surgery for a change of medication and wound examination; return to the clinic 6 to 7 days after surgery for a change of medication and examination of wound healing and recovery. The wound is closed with absorbable sutures, which will gradually fall off after one week. If there are no special circumstances, there is usually no need to change the medication, remove the sutures and cover the sterile gauze afterwards, and you can take a shower and get wet. A warm bath can be started 10 days after surgery.
- You should not do heavy work and avoid strenuous exercise for one week after surgery; however, light work is fine and you can engage in other light daily activities.
- It takes about 3-6 months for the surgical wound and tissues to recover like other normal tissues. More strenuous activities, including ball games, are allowed two weeks after surgery; normal sexual life should not resume until at least one month after surgery. If you have a chronic condition (such as diabetes), you may need a longer recovery period before you can start having sex again and will need to be seen again for re-evaluation.
- In children, the foreskin may sometimes stick to the glans. This will need to be separated during surgery. A few days after surgery, the glans and foreskin will be partially covered with a yellow discharge that will slowly turn into a crust. After a week, new skin will grow underneath and the crust will gradually fall off and the skin will have a normal appearance.
- The surgery will not affect other physical functions or physical health, including penis length, testicular function, ejaculatory function, semen volume, or sperm quality. The pre-surgical condition will be present or absent and will not change as a result of the surgery.
