Microscopic Hernia Repair Surgery Derived from traditional hernia repair surgery with improvements, this procedure uses microscopic surgical techniques. The patient lies flat and receives local anesthesia in the groin area, followed by subcutaneous tissue injections, “genitofemoral nerve branch blockade” and “ilioinguinal nerve blockade” procedures. During surgery, a small incision is made on the skin above the external ring of the groin at a proper position parallel to Langer’s line, a line of collagen fibers in the skin, to reduce the chance of post-operative scar tissue formation. Careful dissection is performed while preserving visible vessels and nerves, until the spermatic cord is separated and turned out.
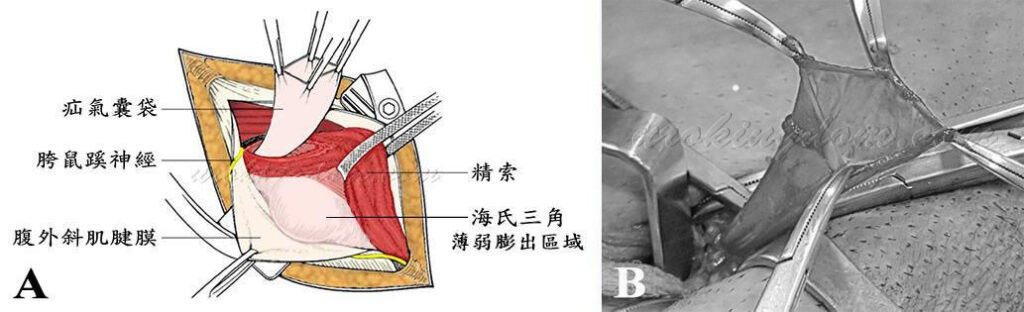
Hernias in children are mostly indirect, which makes treatment easier than direct hernias. However, since the hernia sac wall is weak, it needs to be handled with great care to avoid rupture (Figure 1). After carefully dissecting the hernia sac away from the spermatic cord, the tubular channel near the opening to the abdominal cavity is tied and the hernia sac is removed, without the need to repair the abdominal wall (the posterior wall of the groin), leading to a low recurrence rate (Figure 2).
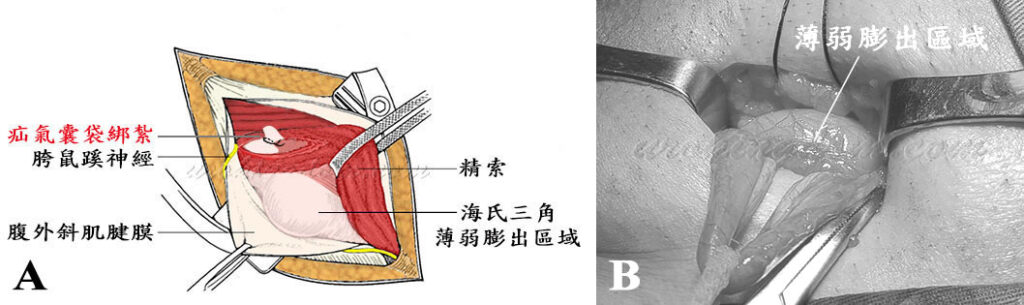
In adult groin hernias, indirect and direct hernias may occur simultaneously. In addition to stripping the hernia sac, if the abdominal wall (groin posterior wall) is weak (Figure 2), an artificial mesh is simultaneously used to repair the wall to strengthen its toughness (Figure 3). This is a recent development in tension-free hernia repair surgery using artificial mesh to reduce tension at the suture site, minimize postoperative pain and reduce recurrence rates (approximately 1-5%), which is lower than that of traditional surgery (10-15%).
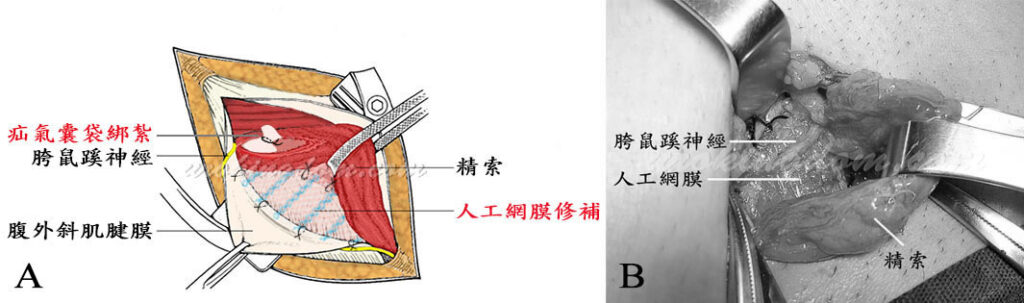
During surgery, the ilioinguinal nerve must be protected to avoid damage (Figure 3A). If there is minor bleeding, electrocautery is not used; instead, a fine suture is used to tie off the bleeding point. Finally, the ilioinguinal nerve is repositioned (Figure 3B), and the flipped-out spermatic cord is returned to its original position. The subcutaneous tissue and skin incisions are sutured layer by layer with absorbable sutures, and the wound is covered with gauze to complete the surgery.
Precise surgery removes only the hernia sac, leaving as much subcutaneous tissue as possible to avoid damage to other tissues, blood vessels and nerves, resulting in minimal bleeding. Due to the presence of blood vessels and nerves near the incision, the use of electrocautery during surgery may damage adjacent blood vessels, nerves or surrounding tissues, resulting in abnormal nerve sensation, numbness, local ischemic necrosis or poor wound healing.
Many medical literature reports have pointed out that the use of electrocautery during surgery destroys local tissue, and the burned area lacks blood circulation, reducing resistance to bacteria and increasing the probability of wound inflammation and infection. Even without infection, it can also affect wound healing.
Microscopic hernia repair surgery completely eliminates the need for electrocautery, resulting in minimal damage to nerve and blood vessels and minimal bleeding. This is the safest and least problematic method.
Not only microscopic hernia repair surgery, but also other related surgeries we perform, including microscopic low ligation of the spermatic vein for the treatment of varicocele, microscopic circumcision, penile vein excision, correction of penile curvature, and penile implant surgery, all follow this principle to minimize the risk of complications.
Advantages of Hernia Repair under Local Anesthesia
- Innovative dual local anesthesia with long-lasting effects that can last for several hours after surgery.
- Laparoscopic surgical techniques are used during surgery, which takes about 1-2 hours.
- Small incisions are made parallel to the blue grid line, reducing the probability of scar tissue formation after surgery.
- Minimal damage is done to nerves, blood vessels, and other tissues, preserving the normal tissue structure.
- Minimal bleeding occurs, and electrocautery is not used to stop bleeding.
- The surgical incision is flat and neat, and the wound heals smoothly and beautifully.
- The surgery can reduce the discomfort caused by abdominal pain due to hernia protrusion.
Precautions for Hernia Repair under Local Anesthesia
- Prior to surgery, a pre-operative evaluation by a physician is necessary to determine if laparoscopic hernia repair is suitable for the patient.
- The innovative dual local anesthesia used during the surgery has a long-lasting effect that can last for 4-6 hours. The surgical procedure is painless and patients can go home after surgery without being hospitalized. After the anesthesia wears off, some discomfort and pain may occur at the surgical site. Patients are advised to take anti-inflammatory and pain medication as prescribed to reduce the pain and discomfort. Generally, the pain gradually decreases after the first night.
- Smoking or exposure to secondhand smoke can affect wound healing and tissue recovery, so it should be avoided as much as possible.
- There may be minor bleeding, bruising, and swelling of the scrotum or foreskin after surgery, which usually resolves on its own.
- Within 7 days after surgery, patients are advised to keep the wound dry and avoid getting it wet. Patients should return to the clinic 2-3 days after the surgery for wound dressing changes and examination. They should return to the clinic 6-7 days after the surgery for further examination of wound healing and recovery. The wound is closed with absorbable sutures and the stitches will gradually fall off after one week. There is usually no need to change dressing or remove sutures after that. Patients can take a bath after 10 days.
- To prevent constipation, patients are advised to drink plenty of water and eat fiber-rich foods such as vegetables and fruits.
- Patients can resume light activities gradually 2 days after surgery. However, they should avoid strenuous activities that involve abdominal exertion, such as coughing, crying, squatting, straining during bowel movements, or lifting heavy objects, within two months after surgery. They should also avoid intense physical activity during this period.
- It takes approximately 3-6 months for the surgical wound and tissue to recover to the same level as other normal tissues. Patients can attempt to resume normal sexual activities after at least one month. If patients have a chronic illness (such as diabetes), the recovery period may be longer, and a follow-up visit is necessary to evaluate their recovery progress.
- The surgery will not affect other physiological functions or body health, including penis length, testicular function, ejaculation function, semen volume, and sperm quality. The patient’s preoperative status remains unchanged after the surgery.
